Shock waves are acoustic pulses that have been used in medicine since the 1980s to treat various conditions, including kidney stones. A particular area of application is Neurology, where we refer to the use of shock waves on the brain as Transcranial Pulse Stimulation (TPS).
In the following section, we would like to familiarise you with the fascinating topic of shock waves in medicine and explore the history, physics and mode of action of this technology.
Shock Waves in Nature
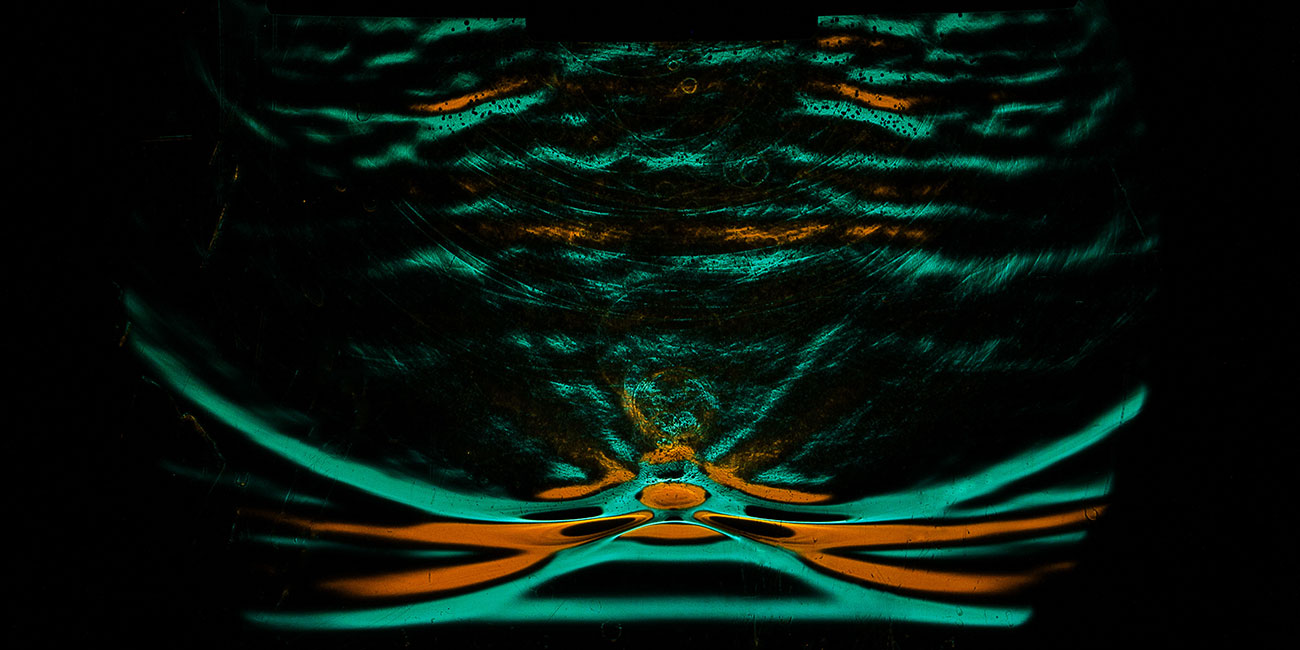
Shock waves are a fascinating phenomenon found throughout nature. They occur when an object moves faster than the speed of sound in a medium (such as air or water), creating a sudden and significant change in pressure, temperature, and density. These waves can be observed in various natural settings.
One of the most common examples of shock waves in the atmosphere is a so-called sonic boom. When an object, such as a jet aircraft, travels faster than the speed of sound, it generates shock waves that propagate through the air, resulting in the characteristic loud boom. Shock waves also occur in thunderstorms. When lightning strikes, it rapidly heats the air around it to extreme temperatures. This causes the air to expand explosively, creating a shock wave that propagates through the atmosphere. As this shock wave travels through the air, it creates a rolling sound that we recognize as thunder.
Another fascinating example of shock waves in nature can be found in the underwater world, courtesy of the pistol crab. Despite their small size, pistol crabs have a remarkable ability to generate shock waves. They do this by snapping their claw at incredible speeds, creating a shock wave that stuns small prey, allowing the crab to capture its meal. The shock wave produced by a pistol crab can even be heard underwater.
The principles behind natural shock waves have found valuable applications in the field of medicine as non-invasive treatment in various medical conditions.
The history and physics of shock waves in medicine
Since the late 1980s, we have used shock waves for the extracorporeal treatment of kidney stones. Today, shock waves are applied in a variety of medical applications in different energy ranges, for example in musculoskeletal disorders and in regenerative medicine. This includes successful applications in diseases of the musculoskeletal system as well as in pseudarthrosis, for stimulating angiogenesis, for wound healing disorders and for treating angina pectoris and heart failure.
Shock waves are acoustic pulses generated mechanically and characterised by a discrete pulse and ultra-short duration. These properties mean that the shock wave does not cause any thermal effects and therefore no tissue heating. They are introduced non-invasively into the body tissue. In order to propagate and be transferred into the body, they require an elastic medium such as water or coupling gel. Shock waves allow physical energy to take effect in localised areas of tissue.
Read more about the physics of shock waves here: What are shock waves? Physics and technology
In Neurology, we refer to shock wave treatment with the NEUROLITH® as Transcranial Pulse Stimulation – TPS for short. The NEUROLITH® has been a CE-marked device since 2018 for treating patients with symptoms of Alzheimer's disease. TPS involves controlled transmission of the pulses through the scalp and skull in a non-invasive manner into the regions of the patient's brain typically affected by Alzheimer's disease.
Read more about TPS here: Transcranial Pulse Stimulation with the NEUROLITH
How do shock waves work?
Mechanotransduction is considered the basic mechanism of shock waves in tissue. It describes the conversion of physical pulses – like shock waves – into cellular processes that are responsible for the positive effects on cell metabolism and the cell cycle.1 This includes migration and differentiation of stem cells, release of nitric oxide (NO)2 as well as stimulation of growth factors (VEGF, BDNF)3,4. This results in the formation of new blood vessels, improvement in blood flow and regeneration of nerves.*
Shock waves vs ultrasound: The most important differences
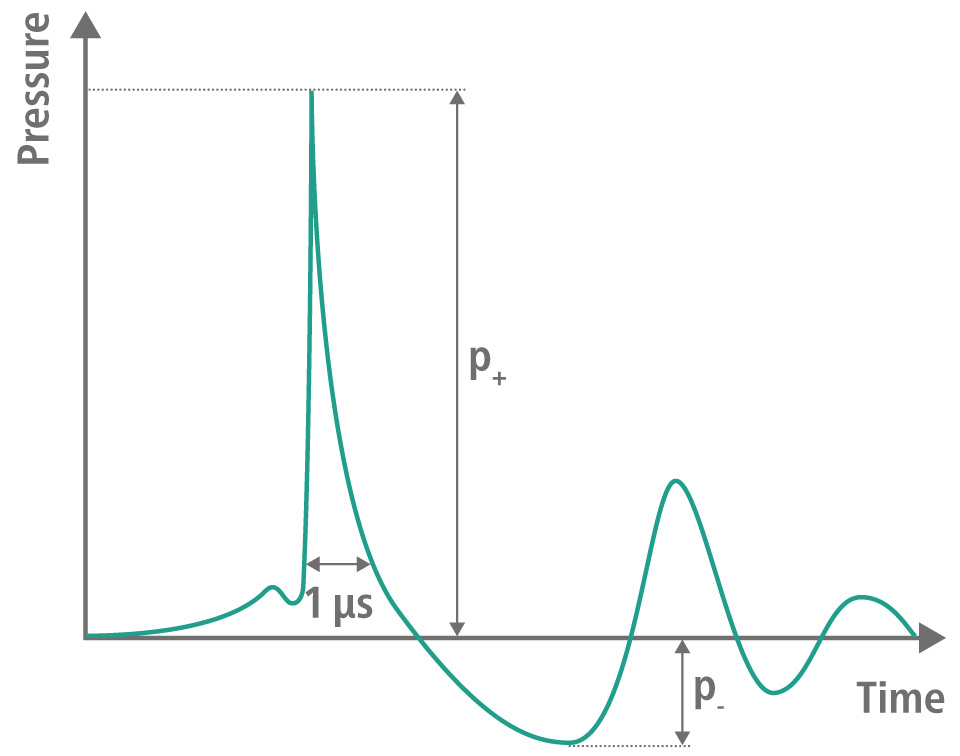
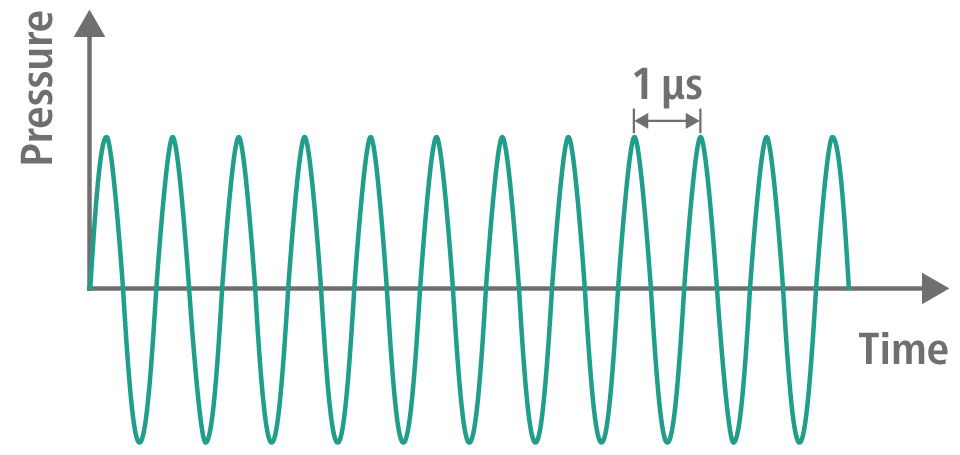
Shock waves and ultrasound waves are both types of sound waves used in medicine. However, there are fundamental differences between the two technologies. Therapeutic ultrasound consists of a continuous wave with numerous oscillations in the megahertz range. In contrast, shock waves consist of a single, very short pressure pulse (1 µs), followed by a tensile wave of lower amplitude (4 – 5 µs). Although both technologies use similar frequencies, they are fundamentally different in nature.
Ultrasound waves can heat tissue with their periodic oscillations, which can be used in a so-called HIFU procedure. Shock waves have a stimulating effect in the low-energy range, whereby heating is not observed.
Due to their different modes of action, shock waves and therapeutic ultrasound pursue different goals in medical applications and are used in different clinical situations due to these differences.
Shock wave
- Single pressure pulse followed by a tensile wave with a relieving effect of lower amplitude
- Asymmetrical pulse form
- No significant tissue heating
- Shock waves are sensed as brief sensory events
- Stimulation of the tissue
Ultrasound
- Continuous wave with numerous oscillations
- Continuous and symmetrical wave form
- The energy is absorbed by tissue, resulting in tissue heating
- Ultrasound waves are not sensed
- Coagulation of the tissue
Unfortunately, scientific publications are repeatedly using the incorrect term »ultrasound« in connection with Transcranial Pulse Stimulation (TPS). TPS actually involves shock waves (acoustic pulse waves), not ultrasound waves.
*The effects stated in connection with shock wave treatments relate to different tissues and cannot be generalised to all indications without scientific evidence.
1 d´Agostino, M. C. et al.: International Journal of Surgery, 24(Pt B):147-153, 2015.
2 Mariotto, S. et al.: Nitric Oxide, 12(2):89-96, 2005.
3 Yahata, K. et al.: Journal of Neurosurgery, 25(6):745-755, 2016.
4 Hatanaka, K. et al.: American Journal of Physiology-Cell Physiology, 311(3):C378-85, 2016.


